The basal-like carcinoma is a recently proposed subtype of breast cancer defined by its gene expression and protein expression profile.[1]
Breast cancer can be divided into five molecular subtypes, including luminal subtype A, luminal subtype B, normal breast-like subtype, HER-2 overexpression subtype) and basal-like subtype.[2] Genotyping fundamentally provides breast cancer patients with improved prognosis and treatment. In all molecular subtypes, basal-like breast cancer (BLBC) is still the biggest challenge in current research due to its strong invasiveness and molecular biological characteristics.
Epidemiology
BLBC is more common among young and premenopausal women in Africa and African Americans.[3][4] Large sample studies based on immunohistochemistry showed that the average age of BLBC patients is 47.7 to 55 years old. Incidence of BLBC and breastfeeding were negative related. Compared with ductal breast cancer, BLBC is more common among women who have earlier menarche age; whose first-term gestational age is less than 26 years old. Women who have low economic and social status, metabolic syndrome and use contraceptives for more than one year are more likely to develop BLBC. Increased waist-hip ratio before menopause also has a significant correlation with BLBC.[5][4]
Treatment and prognosis
Although tumors are often larger and of later stage, basal-like subtypes are more sensitive to anthracycline-based neoadjuvant chemotherapy than luminal breast cancers.[6] Yet, despite initial chemosensitivity, patients with basal-like subtypes have worse distant disease–free survival and overall survival than those with the luminal subtypes,[6] with a 58% 5-year overall survival of people with basal-like carcinoma compared to 88% for those with luminal A subtype.[7] The percentage of patients with minimal residual disease after chemotherapy is higher among basal-like than HER2+/ER− breast cancers.[6] As an independent molecular subtype, BLBC's special biological behavior and poor prognosis is the reason for its significance in the clinical research of breast cancer. BLBC has a high proliferative activity and strong invasiveness, suggesting that it is easier for recurrence and metastasis, and the overall survival period is significantly shortened.[8] BLBC is easier to metastasize to brain and lung through blood vessels, but less to bone and liver, suggesting that tumors have unique metastasis mechanism and once metastasis occurs, the prognosis is very poor. Although many research results need to be further confirmed, evidence suggests BLBC regardless of clinical characteristics or the treatment responses, is a group with heterogeneity.
Molecular pathology
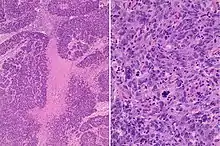
The most common histopathological type is invasive ductal carcinoma. It can also be metaplastic carcinoma, medullary carcinoma and adenoid cystic carcinoma, with high grade, high mitosis count.[9] Central necrosis, apoptotic cells, and stroma lymphocyte reaction and a small amount of interstitial components can be seen through microscopic examination.[10] In BLBC, p53 mutations are usually found and the expression of epidermal growth factor receptor (EGFR or HER-1) and c-KIT are usually positive. Through genetic hybridization techniques, BLBC is verified to have the most complex gene phenotypes. The relationship between BLBC and familial BRCA1-associated breast cancer has been discussed in recent years. Several studies have demonstrated that BRCA1-associated breast cancer is more likely to be a BLBC. However, there are few BRCA1 mutations in BLBC, indicating that it is likely to be epigenetic changes. Studies have reported that the negative regulatory factor of BRCA1 gene, ID4, is often highly expressed in BLBC suggesting that ID4 may play an important role in BLBC. Although the molecular biology mechanisms for BRCA1 and BRCA2 are not understood very well, more and more evidence shows that there are abnormal BRBC1 pathway existing in BLBC.[11]
Proliferation and metastasis
Studies demonstrate that BLBC has a high mitotic index and proliferation ratio. EGFR promotes cell proliferation by activating Ras/MAPK/MAPK pathways. BLBC is characterized by low expression of RB and CyclinD1 gene and high expression of E2F Transcription Factor 3 (E2F-3) as well as Cyclin E genes.[12] The Cyclin D-CDK4/CDK6 complex phosphorylates RB and promotes cell entry into the S phase by releasing the E2F family of transcription factors (inducing CyclinE expression). Additionally, Cyclin E1 is more easily replicated in BLBC than other types of breast cancer, and its expression suggests a poor prognosis.[13] Deletion of RB gene and overexpression of cyclin E play a significant role in the malignant proliferation of BLBC. More and more studies have shown that epithelial-mesenchymal transition (EMT) plays an important role in the invasiveness of breast cancer. EMT refers to the loss of epithelial differentiation characteristics of epithelial cells and shows the characteristics of mesenchymal differentiation, resulting in decreased cell adhesion and increased mobility of cells and allowing cancer cells to obtain infiltration and metastasis.[14] Yang et al.[15] believed that EMT is more likely to occur in BLBC and is stimulated by abnormal microenvironment such as hypoxia. EMT markers such as N-cadherin and vimentin are highly expressed in BLBC, while epithelial markers E-cadherin are often absent.[16] Activation of TGF-β, Wnt, and Notch pathways in BLBC leads to the expression of EMT-related transcription factors FOXC2, Twist, Slug, Snail, and LBX1, and then resulting in down-regulation of E-cadherin and promotion of EMT.[17] Besides, EGFR functions in motility and invasiveness by inducing Twist expression, and thus promoting EMT.[18] It has been reported that EMT in tumors may be accompanied by an increase in neovascularization, which may accelerate the occurrence of hematogenous metastasis in cancer cells.[19] In short, EMT played a crucial role in the transfer of BLBC.
References
- ↑ Livasy CA, Karaca G, Nanda R, Tretiakova MS, Olopade OI, Moore DT, et al. (February 2006). "Phenotypic evaluation of the basal-like subtype of invasive breast carcinoma". Modern Pathology. 19 (2): 264–71. doi:10.1038/modpathol.3800528. PMID 16341146.
- ↑ Kapp AV, Jeffrey SS, Langerød A, Børresen-Dale AL, Han W, Noh DY, et al. (September 2006). "Discovery and validation of breast cancer subtypes". BMC Genomics. 7 (1): 231. doi:10.1186/1471-2164-7-231. PMC 1574316. PMID 16965636.
- ↑ Yang XR, Sherman ME, Rimm DL, Lissowska J, Brinton LA, Peplonska B, et al. (March 2007). "Differences in risk factors for breast cancer molecular subtypes in a population-based study". Cancer Epidemiology, Biomarkers & Prevention. 16 (3): 439–43. doi:10.1158/1055-9965.EPI-06-0806. PMID 17372238.
- 1 2 Millikan RC, Newman B, Tse CK, Moorman PG, Conway K, Dressler LG, et al. (May 2008). "Epidemiology of basal-like breast cancer". Breast Cancer Research and Treatment. 109 (1): 123–39. doi:10.1007/s10549-007-9632-6. PMC 2443103. PMID 17578664.
- ↑ Yang XR, Sherman ME, Rimm DL, Lissowska J, Brinton LA, Peplonska B, et al. (March 2007). "Differences in risk factors for breast cancer molecular subtypes in a population-based study". Cancer Epidemiology, Biomarkers & Prevention. 16 (3): 439–43. doi:10.1158/1055-9965.EPI-06-0806. PMID 17372238.
- 1 2 3 Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, et al. (April 2007). "The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes". Clinical Cancer Research. 13 (8): 2329–34. doi:10.1158/1078-0432.CCR-06-1109. PMID 17438091.
- ↑ Bertucci, F.; Finetti, P.; Birnbaum, D. (2012). "Basal Breast Cancer: A Complex and Deadly Molecular Subtype". Current Molecular Medicine. 12 (1): 96–110. doi:10.2174/156652412798376134. ISSN 1566-5240. PMC 3343384. PMID 22082486.
- ↑ Rakha EA, Reis-Filho JS, Ellis IO (May 2008). "Basal-like breast cancer: a critical review". Journal of Clinical Oncology. 26 (15): 2568–81. doi:10.1200/JCO.2007.13.1748. PMID 18487574.
- ↑ Rakha EA, El-Sayed ME, Green AR, Lee AH, Robertson JF, Ellis IO (January 2007). "Prognostic markers in triple-negative breast cancer". Cancer. 109 (1): 25–32. doi:10.1002/cncr.22381. PMID 17146782.
- ↑ Siziopikou KP, Cobleigh M (February 2007). "The basal subtype of breast carcinomas may represent the group of breast tumors that could benefit from EGFR-targeted therapies". Breast. 16 (1): 104–7. doi:10.1016/j.breast.2006.09.003. PMID 17097880.
- ↑ De Brakeleer S, Bogdani M, De Grève J, Decock J, Sermijn E, Bonduelle M, et al. (June 2007). "Loss of nuclear BRCA1 protein staining in normal tissue cells derived from BRCA1 and BRCA2 mutation carriers". Mutation Research. 619 (1–2): 104–12. doi:10.1016/j.mrfmmm.2007.02.031. PMID 17445839.
- ↑ Gauthier ML, Berman HK, Miller C, Kozakeiwicz K, Chew K, Moore D, et al. (November 2007). "Abrogated response to cellular stress identifies DCIS associated with subsequent tumor events and defines basal-like breast tumors". Cancer Cell. 12 (5): 479–91. doi:10.1016/j.ccr.2007.10.017. PMC 3605202. PMID 17996651.
- ↑ Agarwal R, Gonzalez-Angulo AM, Myhre S, Carey M, Lee JS, Overgaard J, et al. (June 2009). "Integrative analysis of cyclin protein levels identifies cyclin b1 as a classifier and predictor of outcomes in breast cancer". Clinical Cancer Research. 15 (11): 3654–62. doi:10.1158/1078-0432.CCR-08-3293. PMC 2887710. PMID 19470724.
- ↑ Hugo H, Ackland ML, Blick T, Lawrence MG, Clements JA, Williams ED, et al. (November 2007). "Epithelial--mesenchymal and mesenchymal--epithelial transitions in carcinoma progression". Journal of Cellular Physiology. 213 (2): 374–83. doi:10.1002/jcp.21223. hdl:10536/DRO/DU:30007175. PMID 17680632.
- ↑ Yang J, Weinberg RA (June 2008). "Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis". Developmental Cell. 14 (6): 818–29. doi:10.1016/j.devcel.2008.05.009. PMID 18539112.
- ↑ Sarrió D, Rodriguez-Pinilla SM, Hardisson D, Cano A, Moreno-Bueno G, Palacios J (February 2008). "Epithelial-mesenchymal transition in breast cancer relates to the basal-like phenotype". Cancer Research. 68 (4): 989–97. doi:10.1158/0008-5472.CAN-07-2017. PMID 18281472.
- ↑ Storci G, Sansone P, Trere D, Tavolari S, Taffurelli M, Ceccarelli C, Guarnieri T, Paterini P, Pariali M, Montanaro L, Santini D, Chieco P, Bonafé M (January 2008). "The basal-like breast carcinoma phenotype is regulated by SLUG gene expression". The Journal of Pathology. 214 (1): 25–37. doi:10.1002/path.2254. PMID 17973239. S2CID 25174741.
- ↑ Lo HW, Hsu SC, Xia W, Cao X, Shih JY, Wei Y, et al. (October 2007). "Epidermal growth factor receptor cooperates with signal transducer and activator of transcription 3 to induce epithelial-mesenchymal transition in cancer cells via up-regulation of TWIST gene expression". Cancer Research. 67 (19): 9066–76. doi:10.1158/0008-5472.CAN-07-0575. PMC 2570961. PMID 17909010.
- ↑ Niu RF, Zhang L, Xi GM, Wei XY, Yang Y, Shi YR, et al. (September 2007). "Up-regulation of Twist induces angiogenesis and correlates with metastasis in hepatocellular carcinoma". Journal of Experimental & Clinical Cancer Research. 26 (3): 385–94. PMID 17987801.