 | |
| Clinical data | |
|---|---|
| Trade names | Tridione |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | High |
| Metabolism | Demethylated to dimethadione |
| Elimination half-life | 12–24 hours (trimethadione) 6–13 days (dimethadione) |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.004.406 |
| Chemical and physical data | |
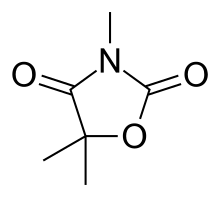
| Formula | C6H9NO3 |
| Molar mass | 143.142 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Trimethadione (Tridione) is an oxazolidinedione anticonvulsant. It is most commonly used to treat epileptic conditions that are resistant to other treatments.
It is primarily effective in treating absence seizures, but can also be used in refractory temporal lobe epilepsy. It is usually administered 3 or 4 times daily, with the total daily dose ranging from 900 mg to 2.4 g. Treatment is most effective when the concentration of its active metabolite, dimethadione, is above 700 µg/mL. Severe adverse reactions are possible, including Steven Johnson syndrome, nephrotoxicity, hepatitis, aplastic anemia, neutropenia, or agranulocytosis. More common adverse effects include drowsiness, hemeralopia, and hiccups.[1][2]
Fetal trimethadione syndrome
If administered during pregnancy, fetal trimethadione syndrome may result causing facial dysmorphism (short upturned nose, slanted eyebrows), cardiac defects, intrauterine growth restriction (IUGR), and mental retardation. The fetal loss rate while using trimethadione has been reported to be as high as 87%.[3]
References
- ↑ American Medical Association Dept of Drugs (1977). AMA Drug Evaluations (3rd ed.). Littleton, Mass.: Pub. Sciences Group. p. 466. ISBN 978-0-88416-175-2. OCLC 1024170745.
- ↑ Rodman MJ, Smith DW (1979). Pharmacology and Drug Therapy in Nursing. Lippincott. p. 259. ISBN 978-0-39754-230-7.
- ↑ Teratology and Drug Use During Pregnancy Retrieved January 2007