 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Pamelor, Noritren, Nortrilen, others |
| Other names | Desitriptyline; ELF-101; E.L.F. 101; N-7048 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682620 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | Tricyclic antidepressant (TCA) |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 32–79%[3] |
| Protein binding | 92%[3] |
| Metabolism | Liver |
| Metabolites | 10-E-Hydroxynortriptyline |
| Elimination half-life | 18–44 hours (mean 30 hours)[3] |
| Excretion | Urine: 40%[3] Feces: minor[3] |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.717 |
| Chemical and physical data | |
| Formula | C19H21N |
| Molar mass | 263.384 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Nortriptyline, sold under the brand name Pamelor, among others, is a medication used to treat depression. This medicine is also sometimes used for neuropathic pain, attention deficit hyperactivity disorder (ADHD), smoking cessation and anxiety.[4][5] As with many antidepressants, its use for young people with depression and other psychiatric disorders may be limited due to increased suicidality in the 18–24 population initiating treatment.[5] Nortriptyline is a less preferred treatment for ADHD and stopping smoking.[5] It is taken by mouth.[5]
Common side effects include dry mouth, constipation, blurry vision, sleepiness, low blood pressure with standing, and weakness.[5] Serious side effects may include seizures, an increased risk of suicide in those less than 25 years of age, urinary retention, glaucoma, mania, and a number of heart issues.[5] Nortriptyline may cause problems if taken during pregnancy.[5] Use during breastfeeding appears to be relatively safe.[4] It is a tricyclic antidepressant (TCA) and is believed to work by altering levels of serotonin and norepinephrine.[5][lower-alpha 1]
Nortriptyline was approved for medical use in the United States in 1964.[5] It is available as a generic medication.[4] In 2020, it was the 155th most commonly prescribed medication in the United States, with more than 3 million prescriptions.[6][7]
Medical uses
Nortriptyline is used to treat depression.[8] This medication is in capsule or liquid and is taken by the mouth one to four times a day, with or without food.[8] Usually people are started on a low dose and it is gradually increased.[8] A level between 50 and 150 ng/mL of nortriptyline in the blood generally corresponds with an antidepressant effect.[9]
In the United Kingdom, it may also be used for treating nocturnal enuresis, with courses of treatment lasting no more than three months. It is also used off-label for the treatment of panic disorder, irritable bowel syndrome, migraine prophylaxis and chronic pain or neuralgia modification, particularly temporomandibular joint disorder.[10]
Neuropathic pain
Although not approved by the FDA for neuropathic pain, many randomized controlled trials have demonstrated the effectiveness of TCAs for the treatment of this condition in both depressed and non-depressed individuals. In 2010, an evidence-based guideline sponsored by the International Association for the Study of Pain recommended nortriptyline as a first-line medication for neuropathic pain.[11] However, in a 2015 Cochrane systematic review the authors did not recommend nortriptyline as a first-line agent for neuropathic pain.[12]
Irritable bowel syndrome
Nortriptyline has also been used as an off-label treatment for irritable bowel syndrome (IBS).[13]
Contraindications
Nortriptyline should not be used in the acute recovery phase after myocardial infarction (viz, heart attack).[14] Use of tricyclic antidepressants along with a monoamine oxidase inhibitor (MAOI), linezolid, or IV methylene blue are contraindicated as it can cause an increased risk of developing serotonin syndrome.[15]
Closer monitoring is required for those with a history of cardiovascular disease,[16] stroke, glaucoma, or seizures, as well as in persons with hyperthyroidism or receiving thyroid hormones.
Side effects
The most common side effects include dry mouth, sedation, constipation, increased appetite, blurred vision and tinnitus.[17][18] An occasional side effect is a rapid or irregular heartbeat. Alcohol may exacerbate some of its side effects.[17]
Overdose
The symptoms and the treatment of an overdose are generally the same as for the other TCAs, including anticholinergic effects, serotonin syndrome and adverse cardiac effects. TCAs, particularly nortriptyline, have a relatively narrow therapeutic index, which increase the chance of an overdose (both accidental and intentional). Symptoms of overdose include: irregular heartbeat, seizures, coma, confusion, hallucination, widened pupils, drowsiness, agitation, fever, low body temperature, stiff muscles and vomiting.[8]
Interactions
Excessive consumption of alcohol in combination with nortriptyline therapy may have a potentiating effect, which may lead to the danger of increased suicidal attempts or overdosage, especially in patients with histories of emotional disturbances or suicidal ideation.
It may interact with the following drugs:[19]
- heart rhythm medications such as flecainide (Tambocor), propafenone (Rhythmol), or quinidine (Cardioquin, Quinidex, Quinaglute)
- cimetidine
- guanethidine
- reserpine
Pharmacology
Nortriptyline is a strong norepinephrine reuptake inhibitor and a moderate serotonin reuptake inhibitor. Its pharmacologic profile is as the table shows with (inhibition or antagonism of all sites).[20][21]
Pharmacodynamics
| Site | Ki (nM) | Species | Ref |
|---|---|---|---|
| SERT | 15–18 | Human | [22][23] |
| NET | 1.8–4.4 | Human | [22][23] |
| DAT | 1,140 | Human | [22] |
| 5-HT1A | 294 | Human | [24] |
| 5-HT2A | 5.0–41 | Human/rat | [25][24] |
| 5-HT2C | 8.5 | Rat | [25] |
| 5-HT3 | 1,400 | Rat | [26] |
| 5-HT6 | 148 | Rat | [27] |
| α1 | 55 | Human | [24] |
| α2 | 2,030 | Human | [24] |
| β | >10,000 | Rat | [28] |
| D2 | 2,570 | Human | [24] |
| H1 | 3.0–15 | Human | [29][24][30] |
| H2 | 646 | Human | [29] |
| H3 | 45,700 | Human | [29] |
| H4 | 6,920 | Human | [29] |
| mACh | 37 | Human | [24] |
| M1 | 40 | Human | [31] |
| M2 | 110 | Human | [31] |
| M3 | 50 | Human | [31] |
| M4 | 84 | Human | [31] |
| M5 | 97 | Human | [31] |
| σ1 | 2,000 | Guinea pig | [32] |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | |||
Nortriptyline is an active metabolite of amitriptyline by demethylation in the liver. Chemically, it is a secondary amine dibenzocycloheptene and pharmacologically it is classed as a first-generation antidepressant.[33]
Nortriptyline may also have a sleep-improving effect due to antagonism of the H1 and 5-HT2A receptors.[34] In the short term, however, nortriptyline may disturb sleep due to its activating effect.
In one study, nortriptyline had the highest affinity for the dopamine transporter among the TCAs (KD = 1,140 nM) besides amineptine (a norepinephrine–dopamine reuptake inhibitor), although its affinity for this transporter was still 261- and 63-fold lower than for the norepinephrine and serotonin transporters (KD = 4.37 and 18 nM, respectively).[22]
Pharmacokinetics
Pharmacogenetics
Nortriptyline is metabolized in the liver by the hepatic enzyme CYP2D6, and genetic variations within the gene coding for this enzyme can affect its metabolism, leading to changes in the concentrations of the drug in the body.[35] Increased concentrations of nortriptyline may increase the risk for side effects, including anticholinergic and nervous system adverse effects, while decreased concentrations may reduce the drug's efficacy.[36][37][38]
Individuals can be categorized into different types of CYP2D6 metabolizers depending on which genetic variations they carry. These metabolizer types include poor, intermediate, extensive, and ultrarapid metabolizers. Most individuals (about 77–92%) are extensive metabolizers,[38] and have "normal" metabolism of nortriptyline. Poor and intermediate metabolizers have reduced metabolism of the drug as compared to extensive metabolizers; patients with these metabolizer types may have an increased probability of experiencing side effects. Ultrarapid metabolizers use nortriptyline much faster than extensive metabolizers; patients with this metabolizer type may have a greater chance of experiencing pharmacological failure.[36][37][38]
The Clinical Pharmacogenetics Implementation Consortium recommends avoiding nortriptyline in persons who are CYP2D6 ultrarapid or poor metabolizers, due to the risk of a lack of efficacy and side effects, respectively. A reduction in starting dose is recommended for patients who are CYP2D6 intermediate metabolizers. If use of nortriptyline is warranted, therapeutic drug monitoring is recommended to guide dose adjustments.[38] The Dutch Pharmacogenetics Working Group recommends reducing the dose of nortriptyline in CYP2D6 poor or intermediate metabolizers, and selecting an alternative drug or increasing the dose in ultrarapid metabolizers.[39]
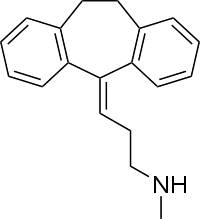
Chemistry
Nortriptyline is a tricyclic compound, specifically a dibenzocycloheptadiene, and possesses three rings fused together with a side chain attached in its chemical structure.[40] Other dibenzocycloheptadiene TCAs include amitriptyline (N-methylnortriptyline), protriptyline, and butriptyline.[40][41] Nortriptyline is a secondary amine TCA, with its N-methylated parent amitriptyline being a tertiary amine.[42][43] Other secondary amine TCAs include desipramine and protriptyline.[44][45] The chemical name of nortriptyline is 3-(10,11-dihydro-5H-dibenzo[a,d]cyclohepten-5-ylidene)-N-methyl-1-propanamine and its free base form has a chemical formula of C19H21N1 with a molecular weight of 263.384 g/mol.[46] The drug is used commercially mostly as the hydrochloride salt; the free base form is used rarely.[46][47] The CAS Registry Number of the free base is 72-69-5 and of the hydrochloride is 894-71-3.[46][47][48]
History
Nortriptyline was developed by Geigy.[49] It first appeared in the literature in 1962 and was patented the same year.[49] The drug was first introduced for the treatment of depression in 1963.[49][50]
Society and culture

Generic names
Nortriptyline is the English and French generic name of the drug and its INN, BAN, and DCF, while nortriptyline hydrochloride is its USAN, USP, BANM, and JAN.[46][47][51][52] Its generic name in Spanish and Italian and its DCIT are nortriptilina, in German is nortriptylin, and in Latin is nortriptylinum.[46][47][51][52]
Brand names
Brand names of nortriptyline include Allegron, Aventyl, Noritren, Norpress, Nortrilen, Norventyl, Norzepine, Pamelor, and Sensoval, among many others.[46][47][52]
Footnotes
- ↑ Nortriptyline actually belongs to a class of drugs called serotonin–norepinephrine reuptake inhibitors (SNRIs). They work at synapse level, and do not allow reuptake of both serotonin and norepinephrine by the neurons. This increases the amount of these neurotransmitters at synpase. In a way, that is not completely clear, this reduces the transmission of pain signals to the brain. It is for this reason, that SNRIs would work in neuropathic pain, but not in nociceptive pain.
References
- ↑ "Nortriptyline Use During Pregnancy". Drugs.com. 22 June 2020. Retrieved 10 October 2020.
- ↑ Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- 1 2 3 4 5 Lemke TL, Williams DA (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 588–. ISBN 978-1-60913-345-0.
- 1 2 3 British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 374. ISBN 9780857113382.
- 1 2 3 4 5 6 7 8 9 "Nortriptyline Hydrochloride Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 22 March 2019.
- ↑ "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- ↑ "Nortriptyline Hydrochloride - Drug Usage Statistics". ClinCalc. Archived from the original on 8 July 2020. Retrieved 7 October 2022.
- 1 2 3 4 "Nortriptyline". MedlinePlus. National Library of Medicine. Retrieved 6 May 2019.
- ↑ Orsulak PJ (September 1989). "Therapeutic monitoring of antidepressant drugs: guidelines updated". Therapeutic Drug Monitoring. 11 (5): 497–507. doi:10.1097/00007691-198909000-00002. PMID 2683251.
- ↑ Sweetman SC, ed. (2002). Martindale. The complete drug reference (33 ed.). Pharmaceutical Press. ISBN 0-85369-499-0.
- ↑ Dworkin RH, O'Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, et al. (March 2010). "Recommendations for the pharmacological management of neuropathic pain: an overview and literature update". Mayo Clinic Proceedings. 85 (3 Suppl): S3-14. doi:10.4065/mcp.2009.0649. PMC 2844007. PMID 20194146.
- ↑ Derry S, Wiffen PJ, Aldington D, Moore RA (January 2015). "Nortriptyline for neuropathic pain in adults". The Cochrane Database of Systematic Reviews. 1 (1): CD011209. doi:10.1002/14651858.CD011605. PMC 6485407. PMID 25569864.
- ↑ "The Use of Antidepressants in the Treatment of Irritable Bowel Syndrome and Other Functional GI Disorders" (PDF).
- ↑ "Nortriptyline label" (PDF). FDA. 2014.
- ↑ Merwar G, Saadabadi A (2018). "Nortriptyline". StatPearls. StatPearls Publishing. PMID 29489270. Retrieved 2018-10-03.
- ↑ Bardai A, Amin AS, Blom MT, Bezzina CR, Berdowski J, Langendijk PN, et al. (May 2013). "Sudden cardiac arrest associated with use of a non-cardiac drug that reduces cardiac excitability: evidence from bench, bedside, and community". European Heart Journal. 34 (20): 1506–16. doi:10.1093/eurheartj/eht054. PMID 23425522.
- 1 2 Brayfield A, ed. (9 January 2017). "Nortriptyline Hydrochloride – Martindale: The Complete Drug Reference". MedicinesComplete. Pharmaceutical Press. Retrieved 11 August 2017.
- ↑ "ALLEGRON". TGA eBusiness Services. Arrow Pharma Pty Ltd. 13 October 2016. Retrieved 11 August 2017.
- ↑ "nortriptyline". www.cardiosmart.org. Retrieved 2018-10-03.
- 1 2 Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 14 August 2017.
- ↑ Brunton L, Chabner B, Knollman B. Goodman and Gilman's The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional; 2010.
- 1 2 3 4 Tatsumi M, Groshan K, Blakely RD, Richelson E (1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". Eur. J. Pharmacol. 340 (2–3): 249–58. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- 1 2 Owens MJ, Morgan WN, Plott SJ, Nemeroff CB (1997). "Neurotransmitter receptor and transporter binding profile of antidepressants and their metabolites". J. Pharmacol. Exp. Ther. 283 (3): 1305–22. PMID 9400006.
- 1 2 3 4 5 6 7 Cusack B, Nelson A, Richelson E (1994). "Binding of antidepressants to human brain receptors: focus on newer generation compounds". Psychopharmacology. 114 (4): 559–65. doi:10.1007/bf02244985. PMID 7855217. S2CID 21236268.
- 1 2 Pälvimäki EP, Roth BL, Majasuo H, et al. (1996). "Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor". Psychopharmacology. 126 (3): 234–40. doi:10.1007/bf02246453. PMID 8876023. S2CID 24889381.
- ↑ Schmidt AW, Hurt SD, Peroutka SJ (1989). "'[3H]quipazine' degradation products label 5-HT uptake sites". Eur. J. Pharmacol. 171 (1): 141–3. doi:10.1016/0014-2999(89)90439-1. PMID 2533080.
- ↑ Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR (1993). "Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs". Mol. Pharmacol. 43 (3): 320–7. PMID 7680751.
- ↑ Bylund DB, Snyder SH (1976). "Beta adrenergic receptor binding in membrane preparations from mammalian brain". Mol. Pharmacol. 12 (4): 568–80. PMID 8699.
- 1 2 3 4 Appl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (2012). "Interactions of recombinant human histamine H1R, H2R, H3R, and H4R receptors with 34 antidepressants and antipsychotics". Naunyn Schmiedebergs Arch. Pharmacol. 385 (2): 145–70. doi:10.1007/s00210-011-0704-0. PMID 22033803. S2CID 14274150.
- ↑ Ghoneim OM, Legere JA, Golbraikh A, Tropsha A, Booth RG (2006). "Novel ligands for the human histamine H1 receptor: synthesis, pharmacology, and comparative molecular field analysis studies of 2-dimethylamino-5-(6)-phenyl-1,2,3,4-tetrahydronaphthalenes". Bioorg. Med. Chem. 14 (19): 6640–58. doi:10.1016/j.bmc.2006.05.077. PMID 16782354.
- 1 2 3 4 5 Stanton T, Bolden-Watson C, Cusack B, Richelson E (1993). "Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics". Biochem. Pharmacol. 45 (11): 2352–4. doi:10.1016/0006-2952(93)90211-e. PMID 8100134.
- ↑ Weber E, Sonders M, Quarum M, McLean S, Pou S, Keana JF (1986). "1,3-Di(2-[5-3H]tolyl)guanidine: a selective ligand that labels sigma-type receptors for psychotomimetic opiates and antipsychotic drugs". Proc. Natl. Acad. Sci. U.S.A. 83 (22): 8784–8. Bibcode:1986PNAS...83.8784W. doi:10.1073/pnas.83.22.8784. PMC 387016. PMID 2877462.
- ↑ O'Connor EA, Whitlock EP, Gaynes B, Beil TL (2009). Screening for Depression in Adults and Older Adults in Primary Care: An Updated Systematic Review. Agency for Healthcare Research and Quality (US). PMID 20722174.
- ↑ Thase ME (2006). "Depression and sleep: pathophysiology and treatment". Dialogues in Clinical Neuroscience. 8 (2): 217–26. doi:10.31887/DCNS.2006.8.2/mthase. PMC 3181772. PMID 16889107.
- ↑ Rudorfer MV, Potter WZ (Jun 1999). "Metabolism of tricyclic antidepressants". Cellular and Molecular Neurobiology. 19 (3): 373–409. doi:10.1023/A:1006949816036. PMID 10319193. S2CID 7940406.
- 1 2 Stingl JC, Brockmöller J, Viviani R (Mar 2013). "Genetic variability of drug-metabolizing enzymes: the dual impact on psychiatric therapy and regulation of brain function". Molecular Psychiatry. 18 (3): 273–87. doi:10.1038/mp.2012.42. PMID 22565785. S2CID 20888081.
- 1 2 Kirchheiner J, Seeringer A (Mar 2007). "Clinical implications of pharmacogenetics of cytochrome P450 drug metabolizing enzymes". Biochimica et Biophysica Acta (BBA) - General Subjects. 1770 (3): 489–94. doi:10.1016/j.bbagen.2006.09.019. PMID 17113714.
- 1 2 3 4 Hicks JK, Swen JJ, Thorn CF, Sangkuhl K, Kharasch ED, Ellingrod VL, Skaar TC, Müller DJ, Gaedigk A, Stingl JC (May 2013). "Clinical Pharmacogenetics Implementation Consortium guideline for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants" (PDF). Clinical Pharmacology and Therapeutics. 93 (5): 402–8. doi:10.1038/clpt.2013.2. PMC 3689226. PMID 23486447.
- ↑ Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, Rongen GA, van Schaik RH, Schalekamp T, Touw DJ, van der Weide J, Wilffert B, Deneer VH, Guchelaar HJ (May 2011). "Pharmacogenetics: from bench to byte—an update of guidelines". Clinical Pharmacology and Therapeutics. 89 (5): 662–73. doi:10.1038/clpt.2011.34. PMID 21412232. S2CID 2475005.
- 1 2 Ritsner MS (15 February 2013). Polypharmacy in Psychiatry Practice, Volume I: Multiple Medication Use Strategies. Springer Science & Business Media. pp. 270–271. ISBN 978-94-007-5805-6.
- ↑ Lemke TL, Williams DA (2008). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 580–. ISBN 978-0-7817-6879-5.
- ↑ Cutler NR, Sramek JJ, Narang PK (20 September 1994). Pharmacodynamics and Drug Development: Perspectives in Clinical Pharmacology. John Wiley & Sons. pp. 160–. ISBN 978-0-471-95052-3.
- ↑ Anzenbacher P, Zanger JM (23 February 2012). Metabolism of Drugs and Other Xenobiotics. John Wiley & Sons. pp. 302–. ISBN 978-3-527-64632-6.
- ↑ Anthony PK (2002). Pharmacology Secrets. Elsevier Health Sciences. pp. 39–. ISBN 1-56053-470-2.
- ↑ Cowen P, Harrison P, Burns T (9 August 2012). Shorter Oxford Textbook of Psychiatry. OUP Oxford. pp. 532–. ISBN 978-0-19-162675-3.
- 1 2 3 4 5 6 Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 888–. ISBN 978-1-4757-2085-3.
- 1 2 3 4 5 Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 752–. ISBN 978-3-88763-075-1.
- ↑ "ChemIDplus - 62265-06-9 - AMLRZIZSGSCSHZ-UHFFFAOYSA-N - Desipramine dibudinate - Similar structures search, synonyms, formulas, resource links, and other chemical information".
- 1 2 3 Andersen J, Kristensen AS, Bang-Andersen B, Strømgaard K (2009). "Recent advances in the understanding of the interaction of antidepressant drugs with serotonin and norepinephrine transporters". Chem. Commun. (25): 3677–92. doi:10.1039/b903035m. PMID 19557250.
- ↑ Dart RC (2004). Medical Toxicology. Lippincott Williams & Wilkins. pp. 836–. ISBN 978-0-7817-2845-4.
- 1 2 Morton IK, Hall JM (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 202–. ISBN 978-94-011-4439-1.
- 1 2 3 "Nortriptyline".
External links
- "Nortriptyline". Drug Information Portal. U.S. National Library of Medicine.